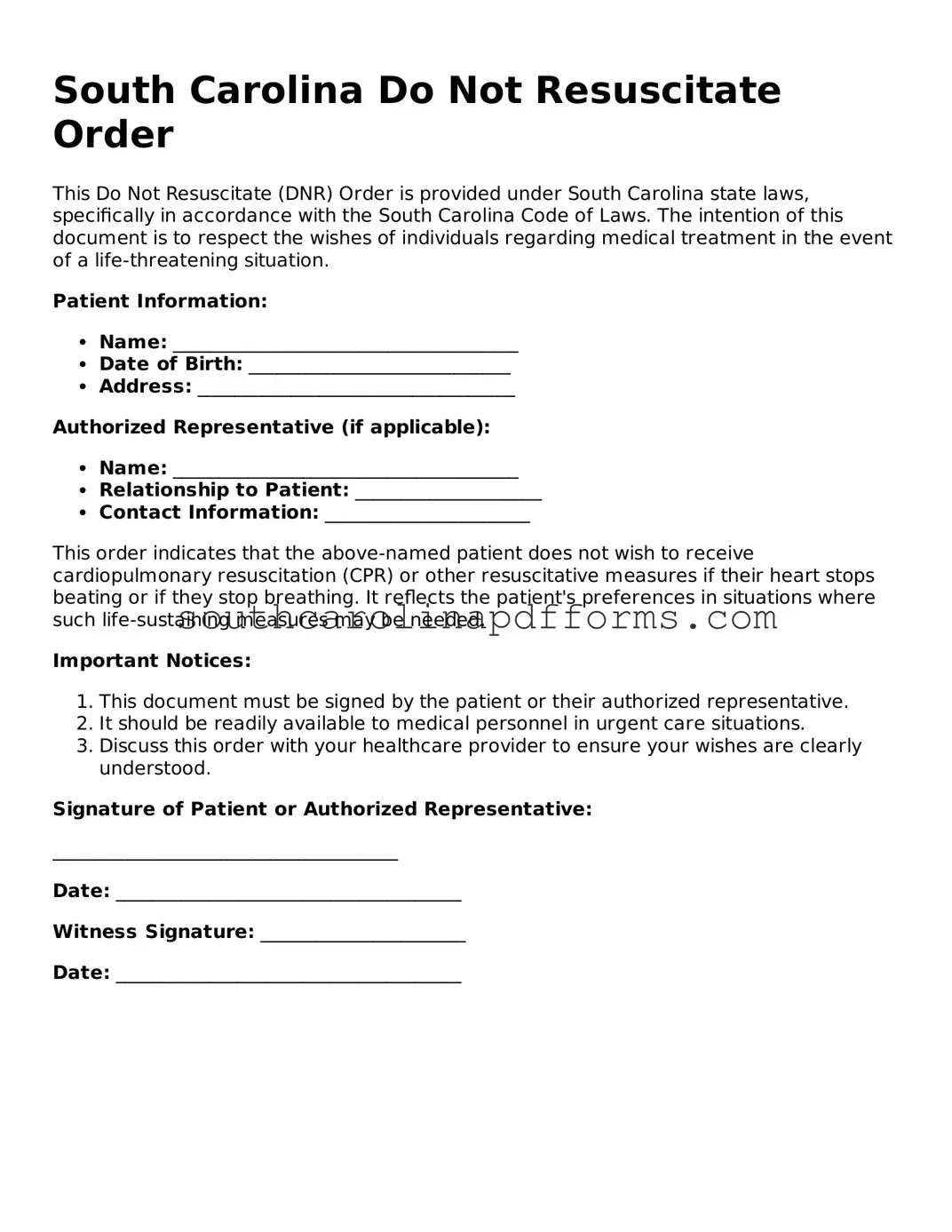
In South Carolina, the Do Not Resuscitate (DNR) Order form serves as a crucial document for individuals who wish to express their preferences regarding medical treatment in emergency situations. This form allows patients to communicate their desire not to receive cardiopulmonary resuscitation (CPR) if their heart stops or they stop breathing. It is essential for ensuring that healthcare providers respect the wishes of patients, particularly those with terminal illnesses or severe medical conditions. The DNR Order must be completed and signed by a physician, reinforcing its validity and ensuring that it meets legal requirements. Additionally, the form should be readily accessible, often kept in a visible location, such as on the refrigerator or in a medical file, so that emergency responders can quickly locate it. Understanding the implications of a DNR Order is vital, as it not only addresses end-of-life care preferences but also encourages meaningful conversations between patients, families, and healthcare providers about treatment options and personal values. In a world where medical interventions can sometimes prolong suffering, the DNR Order empowers individuals to make informed choices about their healthcare journey.